
2025-06-10T13:54:10
Understanding Skin Grafts
- Dermatology
- Family Medicine
- Internal Medicine
- Orthopedics
April 28, 2017 | Family Medicine
Specialties:Family Medicine
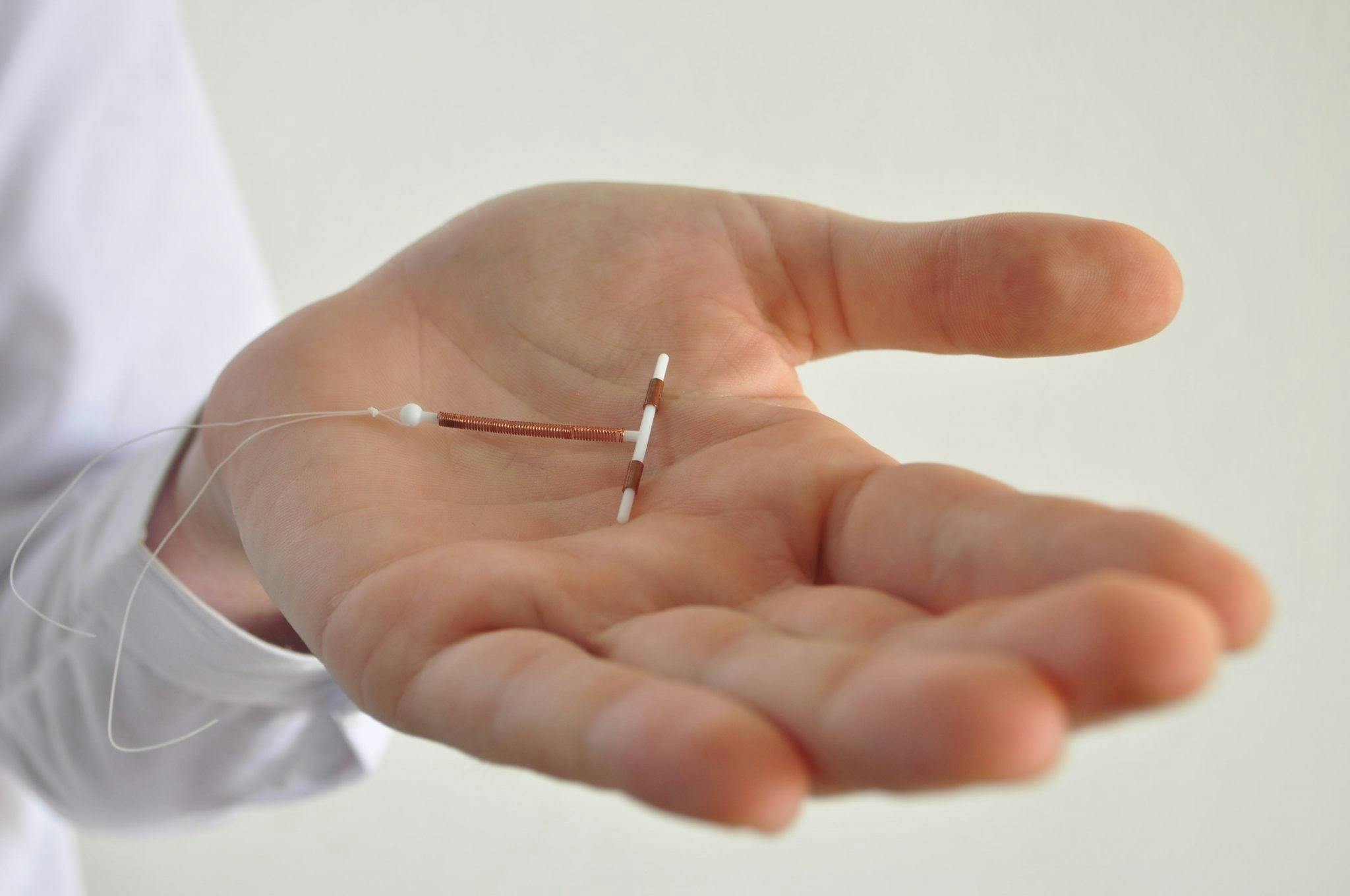
Certain birth control methods involve the insertion of a physical device into the body to prevent pregnancy. One example is an intrauterine device, or IUD. An IUD is a T-shaped device made of plastic, and it’s inserted into the uterus by a doctor.
The goal of an IUD is to prevent the fertilization of female eggs, even if sperm is present in the vagina. IUDs are meant to damage or kill sperm and affect the uterine lining where a fertilized egg would begin developing. There are a couple different types of IUDs, and there are several things you should be aware of if you’re considering one.
Copper IUD: The copper IUD is the most commonly used form of IUD. It works for up to 10 years in a highly effective way and can often be used as emergency contraception if it’s inserted within five days of unprotected sex.
There are several reasons why an IUD might be right for you:
You’re breastfeeding.
You only have a single sex partner, and you’re also that person’s only sex partner. Both of you are infection free, meaning you’re at very low risk for sexually transmitted infections or pelvic inflammatory disease.
You want a long-lasting method of birth control that is easy to insert and can be quickly reversed.
You cannot or do not want to take oral birth control pills, or you are unable to use other hormonal forms of birth control.
There are a few basic risks involved with IUDs:
Menstrual issues: Copper IUDs can increase bleeding or cramps, and lead to spotting between cramps.
Perforation: This is a rare situation in which the IUD becomes stuck in the uterus. It usually occurs during insertion.
Expulsion: Expulsion occurs when the IUD is pushed out of the uterus into the vagina in the first year. It happens in anywhere from 2 to 10 percent of cases.
As long as you’re not pregnant and don’t have any pelvic infections, you’re eligible for an IUD. Your doctor will insert your choice of IUD into your uterus in a process that takes only a few minutes. In some cases, local anesthetic will be used in the area around the cervix. The IUD will contain a plastic string that’s tied to the end and hangs down into the vagina. Your doctor will make sure you can feel the string after insertion, and this is something you’ll want to do every now and then to make sure the IUD is in place.
It’s usually a good idea to have someone with you to drive you home after the procedure. You may go through mild cramping and light bleeding for a couple days after the insertion. For 24 hours after IUD insertion, do not have intercourse, use tampons or insert anything else in the vagina. Your doctor may schedule a follow-up examination to make sure the IUD is in the correct place.
IUDs are extremely effective for birth control. Their success rate is over 99 percent. The majority of pregnancies that occur during IUD use happen because the IUD is expelled from the uterus without the woman noticing.
If you think an IUD might be the right kind of birth control for you, speak to your doctor to find out important details and schedule an appointment.
I practice the full range of family medicine including obstetrics, pediatrics, adolescent medicine and adult medicine. I also practice some orthopedics, remove lumps and bumps, and perform colposcopy, cryotherapy and vasectomies. Due to the volume of deliveries we do, my practice has evolved to be more centered on women and children’s medicine, but I enjoy all aspects of family medicine.
Sources:
“IUD.” Planned Parenthood. https://www.plannedparenthood.org/learn/birth-control/iud
“Intrauterine Device (IUD) for Birth Control.” WebMD. http://www.webmd.com/sex/birth-control/intrauterine-device-iud-for-birth-control
WRITTEN BY:
The Live Better Team

2025-06-10T13:54:10

2025-04-24T14:00:43

2025-03-10T14:24:39

2025-01-21T10:28:42
This information is not intended to replace the advice of a medical professional. You should always consult your doctor before making decisions about your health.