
2023-07-31T14:29:37
What Parents Should Know About Pediatric Neurology: A Neurologist’s Guide to Common Conditions and Treatments
- Neurology
- Pediatrics
May 30, 2017 | Neurology
Specialties:Neurology
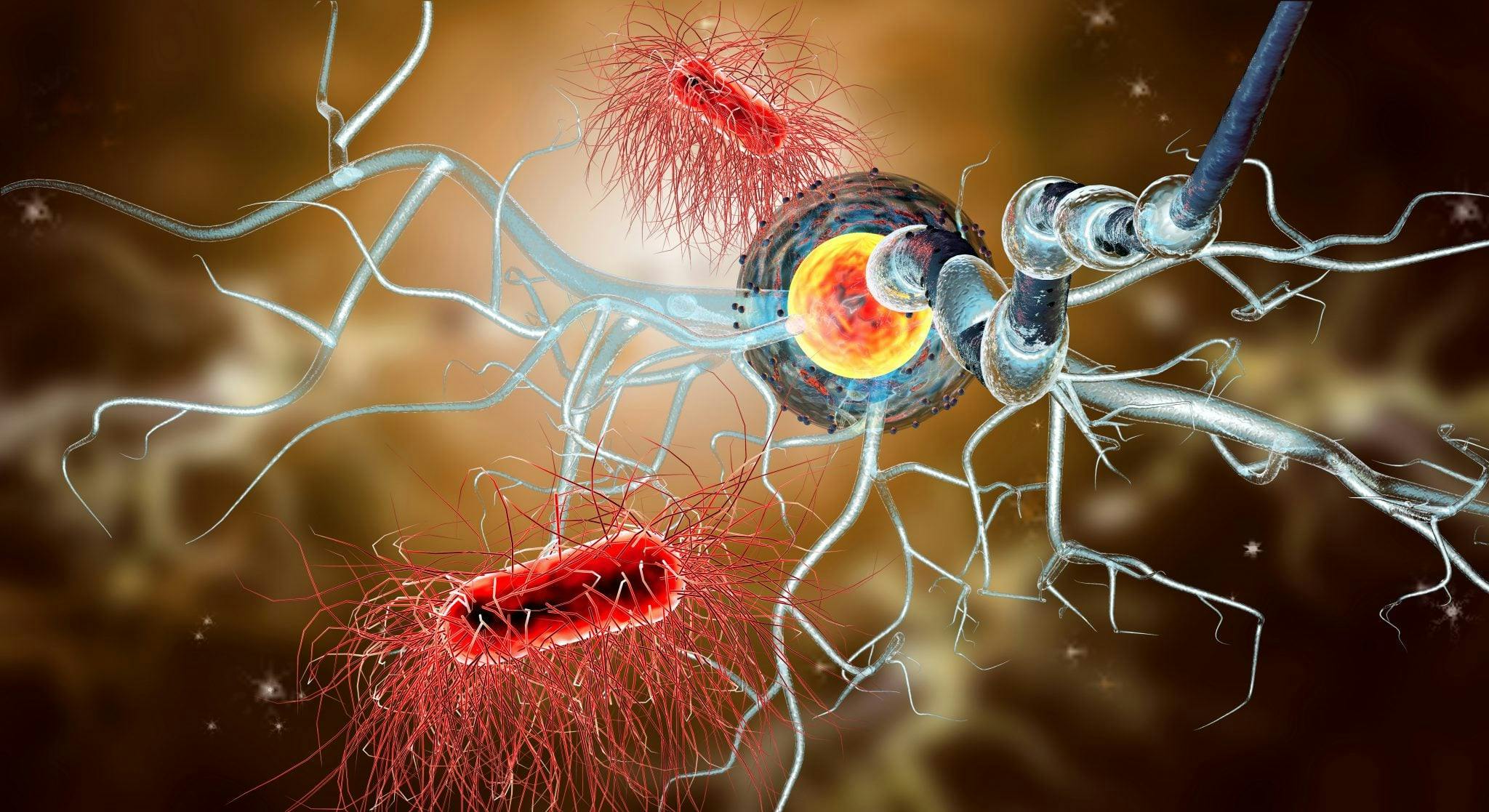
The brain and spinal cord make up the body’s central nervous system, a vital complex of nerve tissues that controls various activities in the body. When the immune system attacks the protective layers of nerve fibers in the central nervous system, this is a disease called multiple sclerosis.
Multiple sclerosis (MS) can lead to the disabling of the brain and spinal cord through nerve deterioration and can cause permanent damage in some cases. There is no cure, though there are various types of treatment that can reduce symptoms for many courses of MS. Here’s the basic information you need to know about multiple sclerosis:
There are four different primary courses, or types, of multiple sclerosis:
Symptoms of multiple sclerosis vary between cases and courses, and they include:
MS patients may also be at risk for the following complications:
The exact cause of MS is unknown. Doctors know that it’s an autoimmune disease where the body’s own immune system attacks myelin, which helps protect nerve fibers. Risk factors for MS include:
If a positive MS diagnosis is found after a series of tests and exams, treatments focus on improving symptoms and slowing the progression of the disease. It also prioritizes speeding up recovery after specific attacks—corticosteroids and plasma exchanges are the two frequent treatments in this area.
For reducing symptoms and modifying progression, a number of different treatments and medications might be used. There are also several basic lifestyle elements that have shown success with reducing symptoms, including exercise, a balanced diet and lowering stress levels.
Like with many chronic illnesses, living day-to-day life with MS can be difficult. Support networks are important, as is continuing to maintain normal activities and recreation. For people struggling, there are support groups available. You can also speak with your doctor about any concerns you have with your MS diagnosis, treatment or management, and he or she will help you determine the best plan for you.
Our neurologists are trained specialists and work with your primary care physicians to develop a treatment plan personalized for you. We have access to the latest in imaging technology and our specialists are up to date on the most recent treatment options.
“What Is MS?” National Multiple Sclerosis Society. http://www.nationalmssociety.org/What-is-MS
“Multiple sclerosis.” The Mayo Clinic. http://www.mayoclinic.org/diseases-conditions/multiple-sclerosis/home/ovc-20131882
WRITTEN BY:
The Live Better Team


2023-07-31T14:29:37

2019-10-15T15:29:00

2019-06-24T09:40:36

2018-06-27T12:00:38
This information is not intended to replace the advice of a medical professional. You should always consult your doctor before making decisions about your health.