
2023-02-15T16:39:02
Understanding Care Coordination & Its Value
- Nephrology
- Value-Based Care
February 22, 2017 | Nephrology
Specialties:Nephrology (Kidney Care)
High blood pressure (also called hypertension) affects 75 percent of American adults. Hypertension can be caused and affected by several diseases and conditions throughout the body, including kidney disease, pregnancy and tumors.
One condition, for example, is called renal hypertension, or renovascular hypertension. This refers to high blood pressure caused by kidney disease or kidney failure. Here are the basics of renal hypertension—its causes, symptoms and forms of treatment.
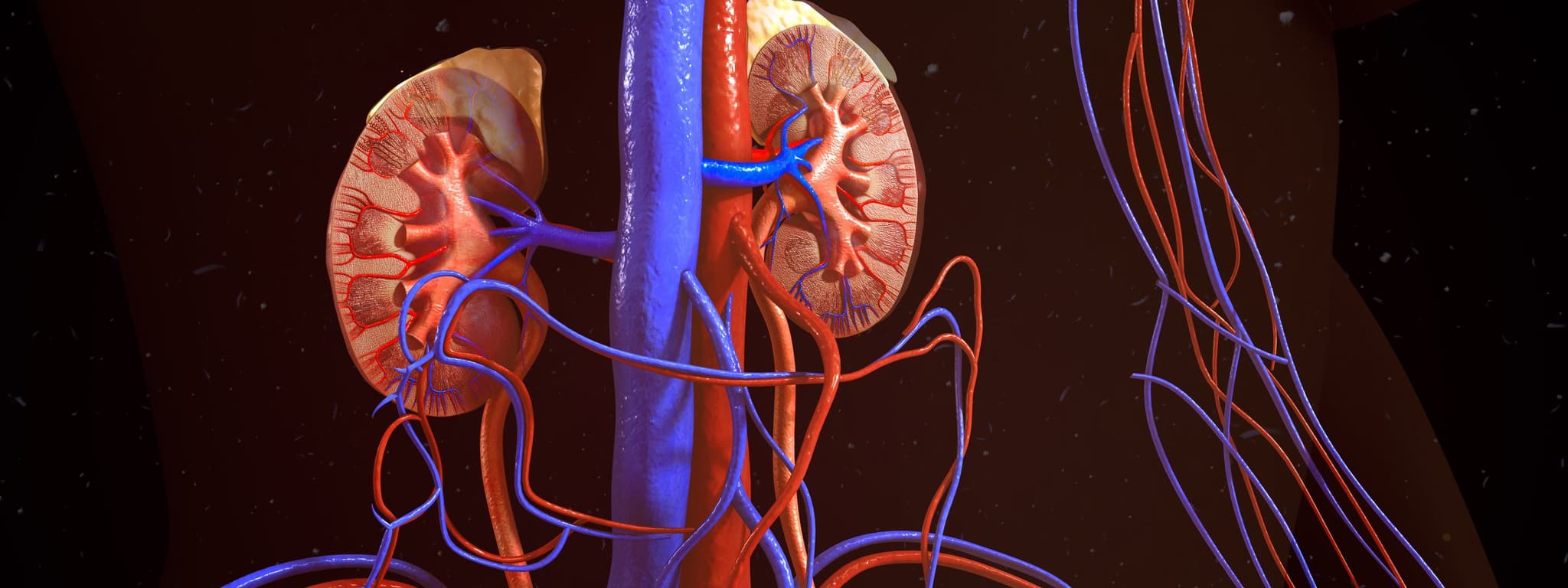
High blood pressure occurs when blood puts too much pressure on artery walls and weakens them. In cases of renal hypertension, the arteries delivering blood to the kidney become narrow, providing lower blood flow.
As a result of the low blood flow, the kidneys respond in the same way that they would respond to dehydration—releasing hormones that help the body retain more sodium and water. The blood vessels then fill with additional fluid, increasing blood pressure.
Most of the time, the narrowing of arteries is caused by atherosclerosis, or hardening of the arteries. It can also be caused by fibromuscular dysplasia, a condition in which arteries develop abnormally.
Like many cases of high blood pressure, renal hypertension often has no noticeable symptoms. This is part of what makes it difficult to recognize, and why blood pressure is such a big part of regular medical check ups. Those with severe renal hypertension may experience the following symptoms:
Renal hypertension is dangerous because it can cause chronic kidney disease, a condition in which symptoms aren’t present until the condition has reached an advanced stage.
Most cases of hypertension are initially treated using medications, and renal hypertension is no different. There are two medications that are most commonly used:
“What is Renal Hypertension?” WebMD. http://www.webmd.com/hypertension-high-blood-pressure/guide/what-is-renal-hypertension#1
“Renovascular Hypertension.” Merck Manual. http://www.merckmanuals.com/professional/cardiovascular-disorders/hypertension/renovascular-hypertension
WRITTEN BY:
The Live Better Team

2023-02-15T16:39:02

2019-10-10T13:34:53

2019-04-03T13:30:08

2018-03-19T11:05:38
This information is not intended to replace the advice of a medical professional. You should always consult your doctor before making decisions about your health.