Value-based Care at Revere Health
We believe we have a responsibility as healthcare providers to lower the cost of care without sacrificing quality.

Healthcare spending in the US is not sustainable
Revere Health recognizes this, and that’s why we’ve made the shift to value-based care. Value-based care isn’t a phase or a fad, it’s where the healthcare industry is heading and it’s the future of medicine. Revere Health’s value-based care efforts have resulted in over $30 million in savings in the last three years alone for our Medicare patients—all while maintaining consistently high quality scores.
Value-based care reverses the rising trend of healthcare costs.
In 1960, each person spent an average of $164 on their healthcare. In 2015, that cost grew to nearly $10,000. If healthcare spending in the U.S. continues at this rate, 100% of all gross domestic product (GDP) will be spent on healthcare by 2040.1
These staggering numbers illustrate the reason why Revere Health decided to become an Accountable Care Organization (ACO) in 2012 and a Next Generation ACO (NGACO) in 2018.
Learn more about our NGACO partnerships
Percent of GDP Spend on Healthcare
1965
1990
2015
2040
- I'm a patient
- I'm a payer
- I'm a provider
- I'm an employer
 What is value-based care?
What is value-based care?
Right now our healthcare system operates mostly as a “fee for service” system, meaning that providers are paid based on the volume of procedures performed or treatments provided, without taking into account whether those things actually improve the outcome for a patient.
Value-based care is the opposite—a system of medicine that focuses on the outcomes instead of the volume of care, ensuring patients get the highest quality care while also focusing on controlling the costs. This approach is designed around patients, with the goal of improving patient health while reducing healthcare costs. It's about getting the right care, in the right place and at the right time.

Value-based care leads to better health outcomes because it encourages patients to play a more dynamic role in their healthcare and promotes preventive care. Data helps providers identify gaps in care like a missed follow-up appointment or screening.

Physicians are actively working to ensure you are receiving low-cost care without sacrificing quality. Data analytics and communication tools help providers navigate the best path for your situation so that you are getting the best value out of your healthcare dollar.

A lower cost of care doesn't matter if you aren't also receiving the best possible care. In a value-based care model, physicians are measured on the quality of care they provide and how well they coordinate and manage your care. It benefits you as a patient—and them as physicians—to provide the best patient care.
 Why does value-based care matter?
Why does value-based care matter?
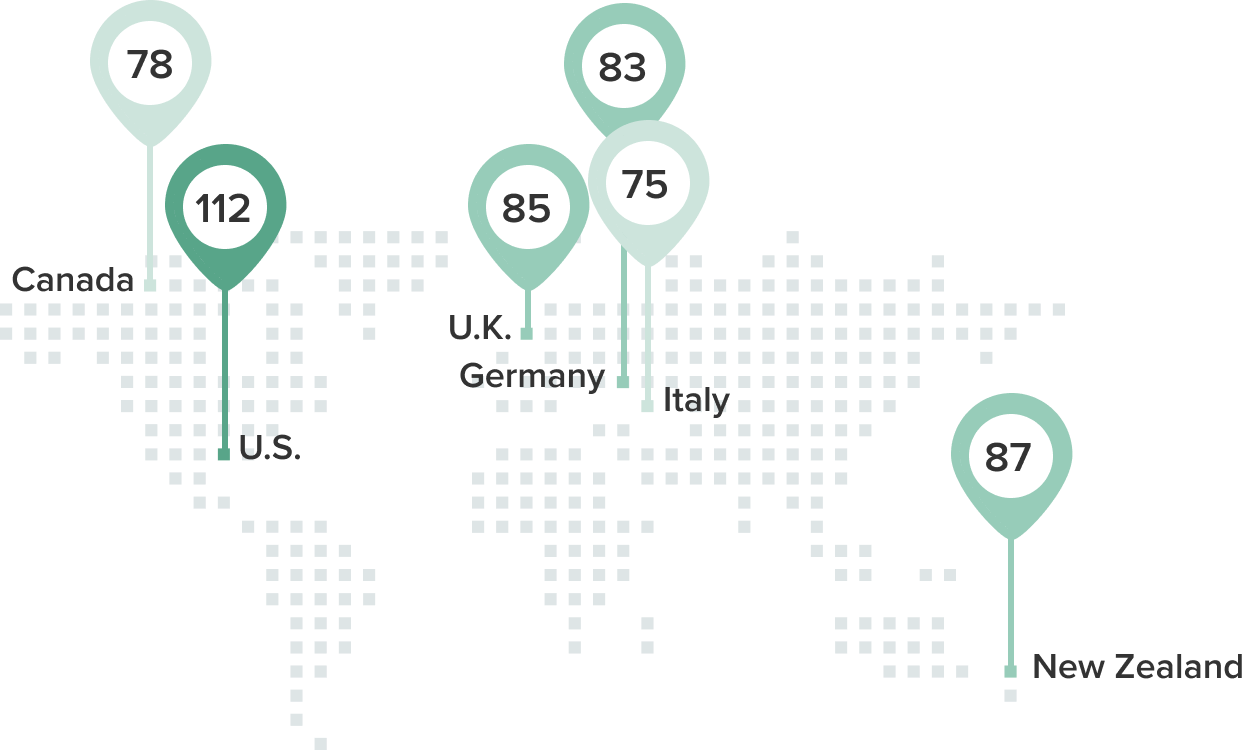
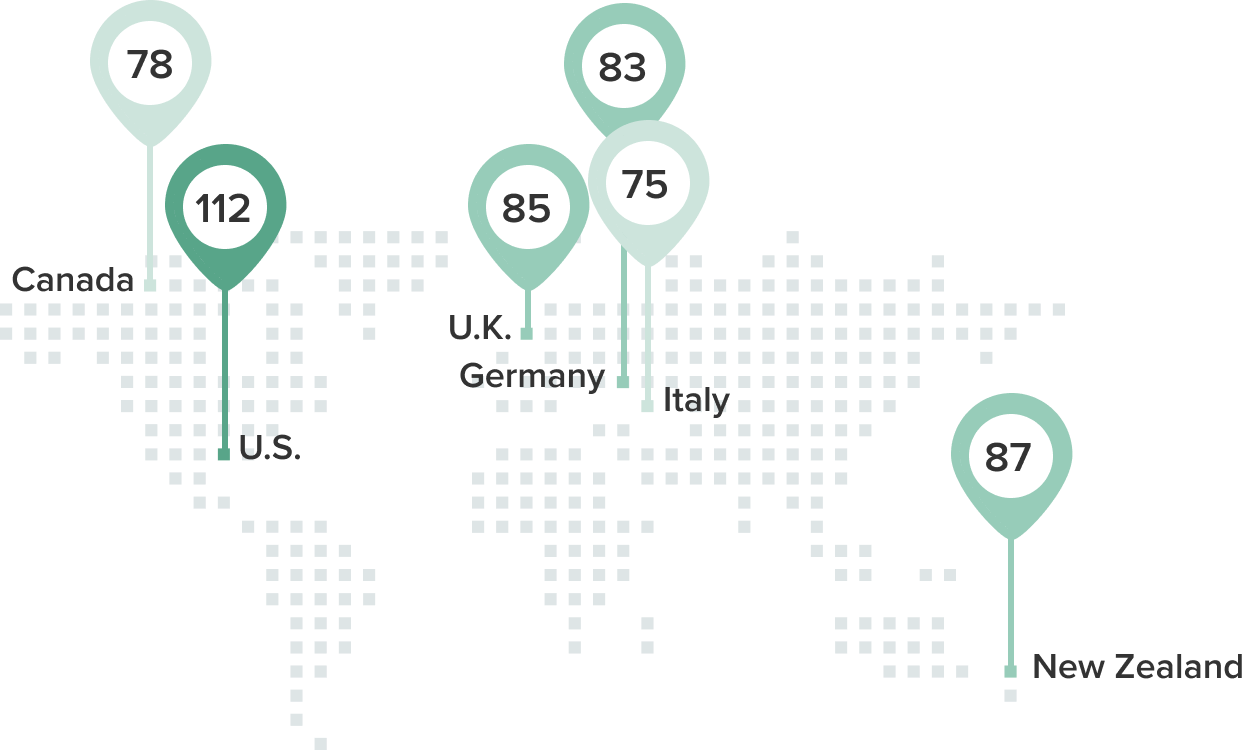
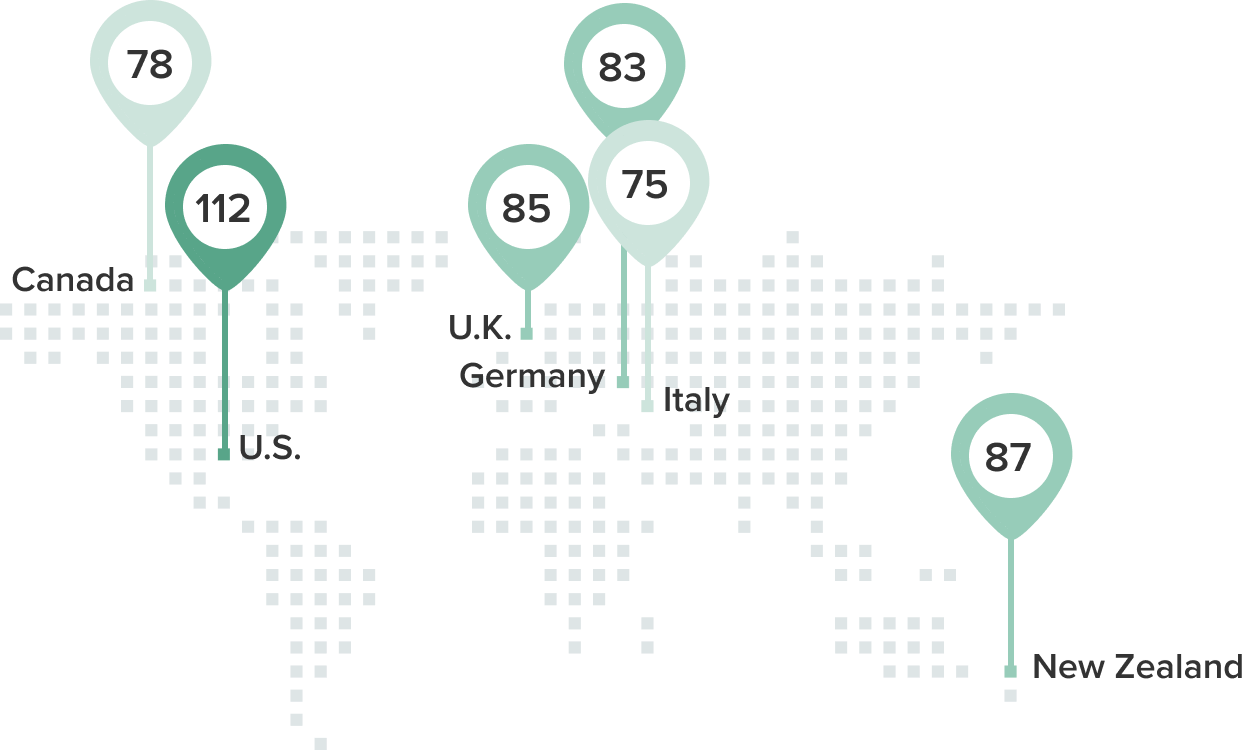
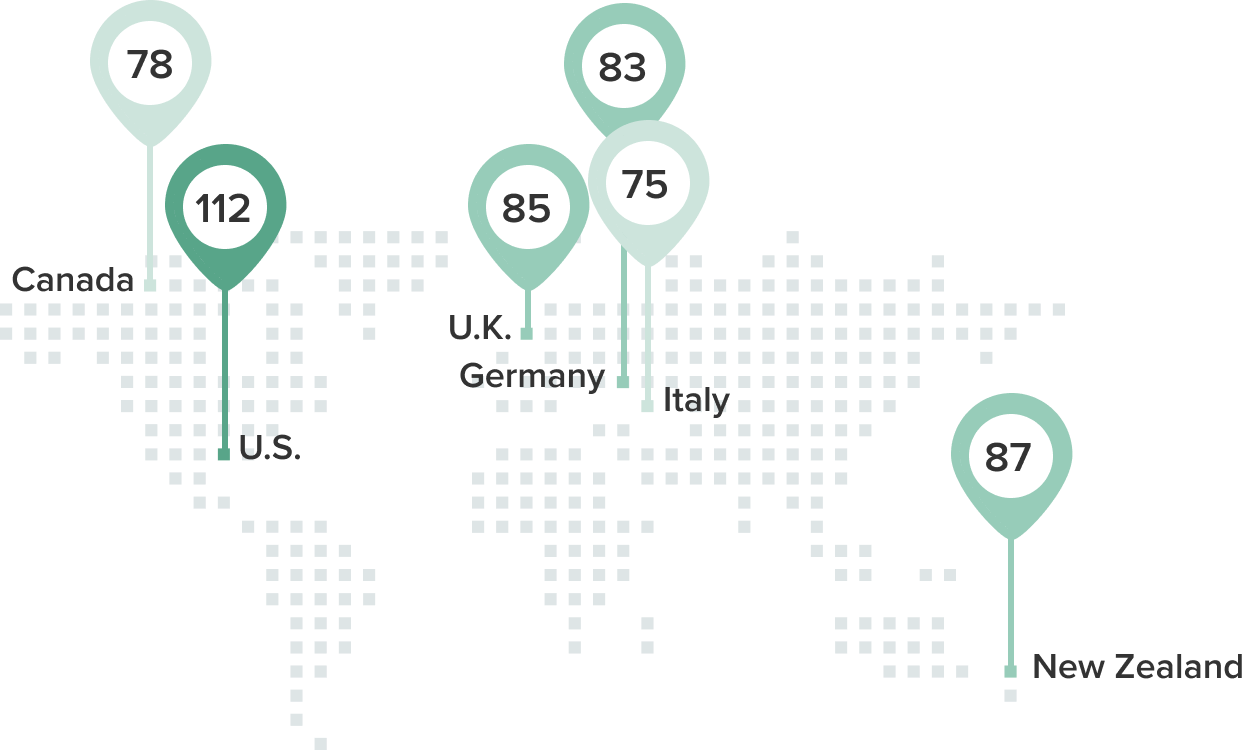
The United States spends up to three times as much on healthcare per capita as other nations with comparable incomes, but the U.S. still has a lower life expectancy, more chronic disease diagnoses and poorer health outcomes. 1
Lower life expectancy
The United States has a significantly lower life expectancy than other countries that spend less on healthcare
More preventable deaths
More people die of preventable diseases and complications in the U.S. than in any other developed nation. *
Highest health costs
The United States spends more money per person on healthcare than any other nation with comparable incomes.
 How does value-based care benefit me?
How does value-based care benefit me?
The idea behind value-based care is simple: improve the quality of healthcare while simultaneously reducing costs. Healthcare organizations around the country, including outpatient clinics, hospitals and insurance providers, have been making the shift to value-based care over the past several years, and many patients are now seeing the effects of this shift.Read more
 Frequently Asked Questions
Frequently Asked Questions
Q: If healthcare costs less, does that mean the quality of care isn't as good?
Q: What can I do to reduce my own healthcare costs?
Q: How do I know as a patient that I'm receiving the best possible care?
Q: How is value-based care different than any other type of care?
Q: Where can I go to make sure I'm getting the best price for my care?
Q: If my insurance covers the cost of my test or procedure, does it really matter where I go for care?
 Tools and Resources
Tools and Resources
Patients have increasing access to different tools that help them navigate the ever-changing landscape of healthcare. Are you taking advantage of these resources?
Patient Portals
A patient portal is a secure site or app that gives patients access to their medical information anytime, anywhere. Follow My Health (FMH) is Revere Health's patient portal. Patients can use it to view their medical records, refill their prescriptions, document health notes and events, and communicate with their providers.
Follow My Health is a highly beneficial tool to help you stay on top of your healthcare, save time and be healthier.
Log on to Follow My Health or set up your Follow My Health account.
Services and Pricing List
Healthcare is just like any other service industry. You wouldn't sign a loan on a car without knowing the final price, but many patients agree to treatment options without having any idea what the total costs will be. Choosing providers and organizations that are transparent about the cost of their services upfront, and asking for more transparency from healthcare providers that don't make that information readily available, means you can be sure you are getting the best price as a consumer.
You can find pricing for a wide variety of procedures at Revere Health here.
Glossary
Navigating the healthcare industry can be tricky. Use this glossary to better understand your health insurance, know where to go for care and learn about other important health information.
Health and Medication Library
There's a lot of information out there about health and wellness. Use this resource to find thousands of health-related topics—peer-reviewed by doctors—explaining diseases and conditions, diagnoses and treatments, surgeries and procedures, and other wellness and safety information.
You can also use this resource to answer your medication questions.
Search health topics here
Health Information Exchange
Most people get care from more than one provider, and sometimes in more than one health system. If this applies to you, it's important to find care providers that share information with each other electronically. This makes your medical information more accessible and your care more convenient.
See if your provider is part of Utah's Clinical Health Information Exchange (cHIE) here.
Health Savings Account Calculator
A health savings account (HSA) allows you to make tax-free contributions to a medical savings account. HSAs are available to taxpayers in the United States on a high -deductible health plan. You can use the money to cover qualified medical expenses and the money rolls over from year to year. Learn more about HSAs and calculate your savings here.
Ways To Reduce Healthcare Costs
By choosing to make smart healthcare decisions, we have the ability to reverse rising healthcare costs. Below is a downloadable resource with tips to help reduce the cost of your care.
Download 8 Ways To Reduce Healthcare Costs
Note Taking Worksheet
If you need extra help remembering your treatment instructions or the the next steps from your doctor, you may benefit from taking notes during your appointment. Use this sample worksheet if you aren't sure what to write down.
Community Resources
Community resources are available to help you get the care you need. Find links to these resources at 211utah.org and from these Healthcare Hotlines in Utah.
Small Steps to Better Your Health
Even small changes can make a big difference in your physical, mental and financial health.
CLICK HERE for more tips to help you create sustainable change for a healthier 2025.
I'm a patient
 What is value-based care?
What is value-based care?
Right now our healthcare system operates mostly as a “fee for service” system, meaning that providers are paid based on the volume of procedures performed or treatments provided, without taking into account whether those things actually improve the outcome for a patient.
Value-based care is the opposite—a system of medicine that focuses on the outcomes instead of the volume of care, ensuring patients get the highest quality care while also focusing on controlling the costs. This approach is designed around patients, with the goal of improving patient health while reducing healthcare costs. It's about getting the right care, in the right place and at the right time.

Value-based care leads to better health outcomes because it encourages patients to play a more dynamic role in their healthcare and promotes preventive care. Data helps providers identify gaps in care like a missed follow-up appointment or screening.

Physicians are actively working to ensure you are receiving low-cost care without sacrificing quality. Data analytics and communication tools help providers navigate the best path for your situation so that you are getting the best value out of your healthcare dollar.

A lower cost of care doesn't matter if you aren't also receiving the best possible care. In a value-based care model, physicians are measured on the quality of care they provide and how well they coordinate and manage your care. It benefits you as a patient—and them as physicians—to provide the best patient care.
 Why does value-based care matter?
Why does value-based care matter?
The United States spends up to three times as much on healthcare per capita as other nations with comparable incomes, but the U.S. still has a lower life expectancy, more chronic disease diagnoses and poorer health outcomes. 1
Lower life expectancy
The United States has a significantly lower life expectancy than other countries that spend less on healthcare
More preventable deaths
More people die of preventable diseases and complications in the U.S. than in any other developed nation. *
Highest health costs
The United States spends more money per person on healthcare than any other nation with comparable incomes.
 How does value-based care benefit me?
How does value-based care benefit me?
The idea behind value-based care is simple: improve the quality of healthcare while simultaneously reducing costs. Healthcare organizations around the country, including outpatient clinics, hospitals and insurance providers, have been making the shift to value-based care over the past several years, and many patients are now seeing the effects of this shift.Read more
 Frequently Asked Questions
Frequently Asked Questions
Q: If healthcare costs less, does that mean the quality of care isn't as good?
Q: What can I do to reduce my own healthcare costs?
Q: How do I know as a patient that I'm receiving the best possible care?
Q: How is value-based care different than any other type of care?
Q: Where can I go to make sure I'm getting the best price for my care?
Q: If my insurance covers the cost of my test or procedure, does it really matter where I go for care?
 Tools and Resources
Tools and Resources
Patients have increasing access to different tools that help them navigate the ever-changing landscape of healthcare. Are you taking advantage of these resources?
Patient Portals
A patient portal is a secure site or app that gives patients access to their medical information anytime, anywhere. Follow My Health (FMH) is Revere Health's patient portal. Patients can use it to view their medical records, refill their prescriptions, document health notes and events, and communicate with their providers.
Follow My Health is a highly beneficial tool to help you stay on top of your healthcare, save time and be healthier.
Log on to Follow My Health or set up your Follow My Health account.
Services and Pricing List
Healthcare is just like any other service industry. You wouldn't sign a loan on a car without knowing the final price, but many patients agree to treatment options without having any idea what the total costs will be. Choosing providers and organizations that are transparent about the cost of their services upfront, and asking for more transparency from healthcare providers that don't make that information readily available, means you can be sure you are getting the best price as a consumer.
You can find pricing for a wide variety of procedures at Revere Health here.
Glossary
Navigating the healthcare industry can be tricky. Use this glossary to better understand your health insurance, know where to go for care and learn about other important health information.
Health and Medication Library
There's a lot of information out there about health and wellness. Use this resource to find thousands of health-related topics—peer-reviewed by doctors—explaining diseases and conditions, diagnoses and treatments, surgeries and procedures, and other wellness and safety information.
You can also use this resource to answer your medication questions.
Search health topics here
Health Information Exchange
Most people get care from more than one provider, and sometimes in more than one health system. If this applies to you, it's important to find care providers that share information with each other electronically. This makes your medical information more accessible and your care more convenient.
See if your provider is part of Utah's Clinical Health Information Exchange (cHIE) here.
Health Savings Account Calculator
A health savings account (HSA) allows you to make tax-free contributions to a medical savings account. HSAs are available to taxpayers in the United States on a high -deductible health plan. You can use the money to cover qualified medical expenses and the money rolls over from year to year. Learn more about HSAs and calculate your savings here.
Ways To Reduce Healthcare Costs
By choosing to make smart healthcare decisions, we have the ability to reverse rising healthcare costs. Below is a downloadable resource with tips to help reduce the cost of your care.
Download 8 Ways To Reduce Healthcare Costs
Note Taking Worksheet
If you need extra help remembering your treatment instructions or the the next steps from your doctor, you may benefit from taking notes during your appointment. Use this sample worksheet if you aren't sure what to write down.
Community Resources
Community resources are available to help you get the care you need. Find links to these resources at 211utah.org and from these Healthcare Hotlines in Utah.
Small Steps to Better Your Health
Even small changes can make a big difference in your physical, mental and financial health.
CLICK HERE for more tips to help you create sustainable change for a healthier 2025.
I'm a payer
 Why does value-based care matter?
Why does value-based care matter?
The United States spends up to three times as much on healthcare per capita as other nations with comparable incomes, but the U.S. still has a lower life expectancy, more chronic disease diagnoses and poorer health outcomes. 2
Lower life expectancy
The United States has a significantly lower life expectancy than other countries that spend less on healthcare
More preventable deaths
More people die of preventable diseases and complications in the U.S. than in any other developed nation. *
Highest health costs
The United States spends more money per person on healthcare than any other nation with comparable incomes.
 History of value-based care at Revere Health
History of value-based care at Revere Health
Revere Health has participated in quality-based programs since 2005 with many different payer programs, including Medicare Care Management Performance (MCMP), the Physician Quality Reporting Initiative (PQRI) that became the Physician Quality Reporting System, Meaningful Use, clinical-based programs and the Medicare Shared Savings Plan (MSSP).
In 2012, Revere Health, formerly Central Utah Clinic, was the first healthcare group based in Utah to be accredited as an Accountable Care Organization (ACO) by Medicare. We have been building on our success with other commercial payer programs and demonstrated success with MSSP in 2015.
1969
The Clinic is Born
Revere Health, formerly Central Utah Clinic is born in Provo, Utah.
1980
Initial Growth
Central Utah Clinic grows to 15 doctors and 5 specialties including internal medicine, gastroenterology, cardiology, medical oncology and dermatology.
1990
Payson
Internal medicine office expands into Payson.
2002
Orthopedics
Central Utah Clinic welcomes an established orthopedic group in Provo into the practice, further expanding the specialty skill set within the region.
2007
American Fork
The American Fork campus is completed offering residents a wide range quality specialty healthcare and a state of the art surgery center.
2009
Family Practice
The first family practice groups join, initiating an integrated healthcare system beyond specialties.
2010
Southern Utah
Southern Utah specialty groups and family medicine join the Clinic.
2012
Northern Utah
Central Utah Clinic expands into Northern Utah with four groups.
2012
Medicare Accreditation
Revere Health became the first accountable care organization (ACO) in Utah.
2013
Cardiology
Southern Utah adds a region-leading cardiology group.
2013
BYU Orthopedics Partnership
Clinic becomes exclusive orthopedics sports medicine provider for BYU Athletics.
2015
Rebrand
Central Utah Clinic rebrands to become Revere Health.
2016
Salem Campus
Opened Salem multi-specialty health center.
2018
Next Generation ACO
Revere Health becomes the first ACO in Utah accepted into the Next Generation ACO program.
2020
St. George Campus
Opened multi-specialty health center.
1969
1980
1990
2002
2007
2009
2010
2012
2012
2013
2013
2015
2016
2018
2020
 Participating Programs
Participating Programs
I'm a provider
 What is value-based care?
What is value-based care?
 Why does value-based care matter?
Why does value-based care matter?
The United States spends up to three times as much on healthcare per capita as other nations with comparable incomes, but the U.S. still has a lower life expectancy, more chronic disease diagnoses and poorer health outcomes. 2
Lower life expectancy
The United States has a significantly lower life expectancy than other countries that spend less on healthcare
More preventable deaths
More people die of preventable diseases and complications in the U.S. than in any other developed nation. *
Highest health costs
The United States spends more money per person on healthcare than any other nation with comparable incomes.
 How is value-based care different?
How is value-based care different?
 Hear it from your peers
Hear it from your peers
 What does this mean for my patients?
What does this mean for my patients?
When you refer your patients to Revere Health, you can feel confident that your patients are getting the highest quality care at the lowest possible cost. Our patients’ cost of care is driven in part by our ability as providers to work together and determine appropriate care for each patient. Here’s what you can expect when you refer your patient to a Revere Health provider:
Team Care
Our physicians and advanced care practitioners work collaboratively with you and your staff to provide the most efficient and uninterrupted care experience for your patients.
Timely Access
Access to specialty care is at the forefront of our initiatives. Our extensive team of providers in multiple specialties allows patients to see a provider in a timely manner.
Cost Savings
Revere Health has a proven track record in reducing the total cost of care for patients as an Accountable Care Organization. Affordable costs are a priority when you refer your patients to us.
Shared Information
We participate in the Utah Clinical Health Information Exchange (cHIE), allowing us to securely exchange information about our shared patients.
I'm an employer
 What is value-based care?
What is value-based care?
Revere Health started its transition to a value-based model of care over a decade ago in an effort to reduce healthcare spending. While we focus on lowering the cost of healthcare we continue to focus on quality and patient satisfaction. In the last three years alone, Revere Health has reduced healthcare spending for our Medicare population by more than $30 million.
There are many ways to lower healthcare costs and still get the right care at the right place at the right time.
By choosing to make smart healthcare decisions, we have the ability to reverse rising healthcare costs . Employers can especially benefit from smart decision making among their workforce. However, it is important to provide employees with information and actionable steps they can take to aid in this effort. Below is a downloadable resource with tips to help your employees reduce the cost of their care.
We’ll be updating this page with additional tips, resources and information that can help employers and employees understand ways to reduce healthcare costs so check back regularly.
1. Centers for Medicaid and Medicare Services (CMS), National Health Expenditure Data






