
2024-07-02T11:42:04
Growth in Life: A Mental Health Counselor’s Perspective
- Behavioral Health
November 1, 2022 | Behavioral Health
Specialties:Behavioral Health

I recently participated in a podcast with United Way of Utah County, where I had a chance to sit down and visit with Everyday Strong Director Michaelann Gardner. We had a very relaxing discussion on the topic of: “How do I respond to my child’s negative self-talk?” We focused on the early teenage years, but our conversation has a lot of great applications for people of all ages. As soon as it has a chance to be edited, a link will be available.
I fielded a lot of questions about what goes on in therapy sessions and what should or should not be talked about. Here are a few observations I have made over the years related to this topic:
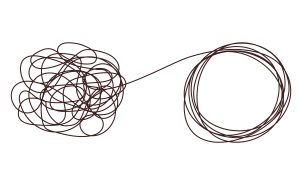
“I apologize for dumping everything on you” or “I’m so sorry for sounding disorganized in everything I just said” are phrases I hear often. These seem to happen on a first visit or when an individual is feeling overwhelmed or weighed down with indecision. It’s appreciated, but not needed. There is no need to apologize for expressing feelings, much less having them. As people talk, I am quietly organizing everything that is being said and triaging the needs of the individual. I feel like the picture below helps illustrate what is happening in the background but not necessarily being seen.
I like to relate our struggles to gas in a propane tank. Whether the tank is completely full or half full, it still occupies the same space. The same can be said for whatever is bothering us. We need a chance to process our experiences. There have been many times when something was shared with me almost as an afterthought, but it turned out to be an incredibly important missing piece to their puzzle. At the same time, I have personally experienced moments when I have ‘catastrophized’ problems that have surfaced in my own life and needed someone to share those thoughts and experiences with.
We don’t just talk about feelings during visits. We talk about experiences and what they mean to individuals and even groups of people, like family members. What does it mean to get married, get divorced, have children, or go off to school? We talk about how behavior is related to our environment and what motivates our behavior. We process local and world events together and talk about how these can change the individual. We talk about the foods we eat, leisure activities, or what we spend our money on. We also discuss chronic, acute, and terminal illnesses because of the direct impact they have on a myriad of issues.
We have a saying, “almost nobody escapes childhood unscathed.” There are a lot of requests for trauma-based therapy, and most therapists are trained in many of these evidence-based interventions. Like many clinicians, I have a strong preference for EMDR treatment as it tends to be more efficient at getting to the root of the trauma. I never like hearing: “Well, others have it worse than me,” because this is a way to minimize what was experienced and delay needed healing. Trauma isn’t limited to veterans returning from combat. Like drops of water that erode a rock, repeated exposure to specific events can have a similar effect. PTSD is one of the most common mental health disorders.
I regularly reassure my patients that there is absolutely no judgment that occurs during the session at all. It really is an honor and privilege when people feel safe and comfortable enough to share details that they may have never shared out loud before. I take this responsibility very seriously. As therapists, we understand that individuals are unique, but problems are no respecter of persons. The inherent difficulties of living are common among all people. During some particularly tough visits, I have been known to personally walk patients out the back door in order to avoid others and help maintain their dignity.
There really is no prescribed amount of time or frequency for someone to come in for services – it is about as unique as the individual. Sometimes, I wish people would come in more frequently and stay longer. There are others who like the ongoing support and reassurance that comes with sharing their experiences. Often, time equals comfort, and that makes for great treatment. Our job is to help patients make independent decisions and then to live with the results.
I try to reassure each person I see that everything that gets said in the office stays in the office, with only a couple of exceptions. Generally, these exceptions include:
Even with these exceptions, I make it a rule to only share what is absolutely necessary for another person or entity to do their job. Being ‘specifically vague’ is my guiding principle in these matters.
Behavioral Health records at Revere Health are only accessible by Providers. The notes that are done in sessions cannot be shared with another person or entity regardless of who requests it, though HIPAA allows for some exceptions. The notes belong to the mental health provider and are only shared at the discretion of the provider. On occasion, I will share what is written during a particular visit with a patient if I think it is beneficial from a therapeutic perspective.
It’s rare that I don’t give out some kind of homework assignment during a visit. My feeling is that the skills that are learned during our visits need to be applied at home to see how they work. Most people, especially kids, are expecting something similar to what is given in school. In reality, my “homework” seldom resembles anything a teacher gives out. I recently gave a homework assignment for a teenage girl to get at least 3 hugs every day. I wanted the hugs to be the big bear hugs and not the side hugs we give acquaintances. She was both surprised and excited to do her “homework” and then to report back about what she learned. She was pleased when her parents were more than willing to help her fulfill this assignment. Both of her parents became the first hugs of each day.
Stream the full EveryDay Strong episode wherever you listen to podcasts.
If you have any concerns about your mental health or the mental health of a loved one you can call Allan Pauole, CMHC, or one of our Revere Health Behavioral Health offices in Utah.
WRITTEN BY:
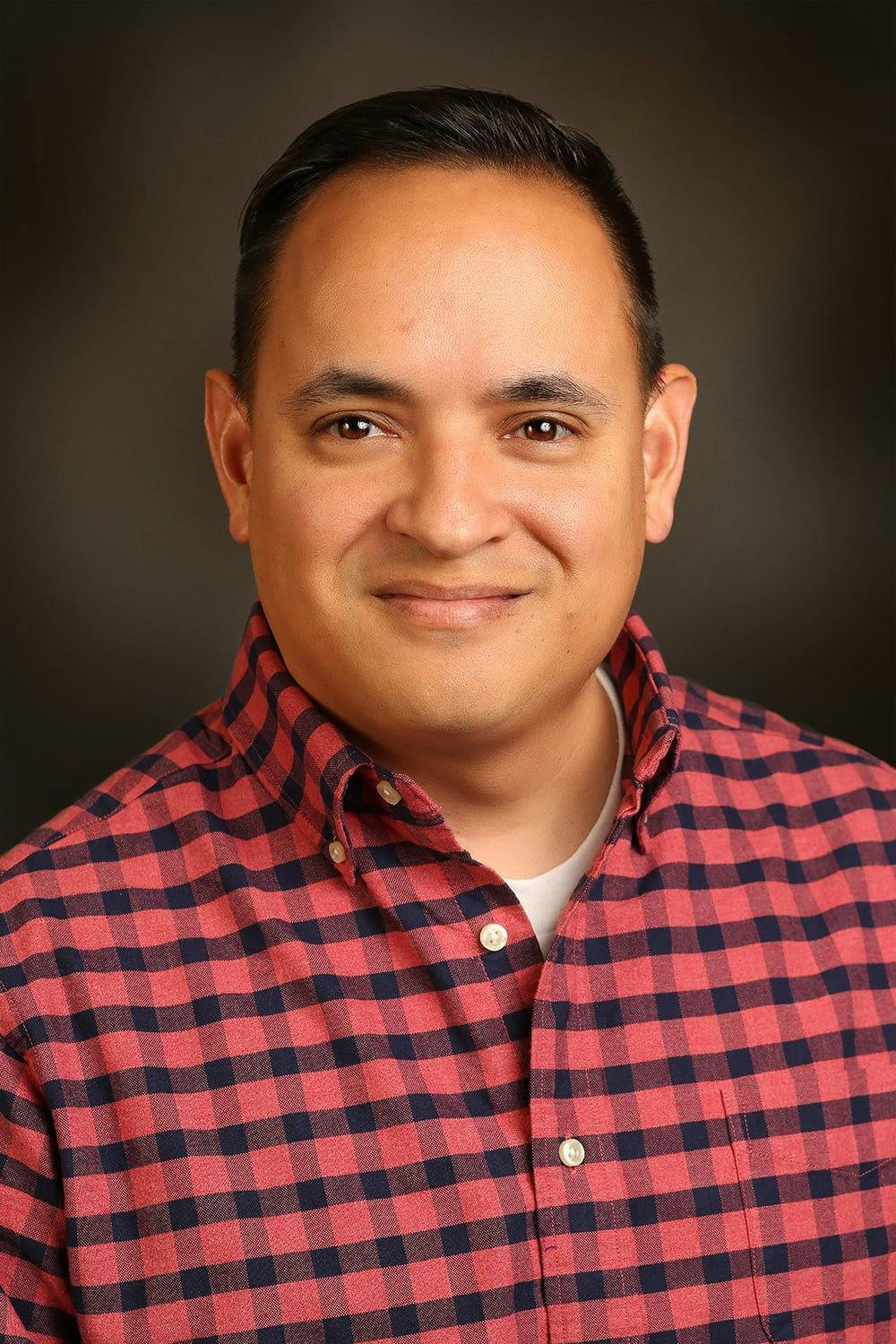
Allan Pauole, CMHC
Allan Pauole is one of our mental health therapists. He has worked for Utah, Juab and Millard counties providing both mental health and substance abuse counseling for hospitals, Utah’s drug court population, and private agencies. Allan also worked for the Paiute Indian Tribe of Utah as a social worker and served as the primary liaison for the tribe in all child custody hearings involving the Division of Child and Family Services and the juvenile courts. He is quite versed in navigating the sometimes dueling interests between the mental health and legal systems. Allan has been a licensed clinical mental health counselor for over 15 years and has extensive training in Motivational Interviewing (MI), Dialectical Behavior Therapy (DBT), substance abuse counseling, and Trauma Focused Cognitive Behavior Therapy(TF-CBT). He is EMDR trained. He is also able to treat all forms of Anxiety, Depression, ADHD, PTSD, and Personality Disorders for patients of all ages. He has an especially strong interest in working with teens and college age adults as he recognizes the challenging and unique transition phase this can be.


2024-07-02T11:42:04

2024-04-09T04:30:04

2024-01-08T11:58:49

2023-10-03T10:37:02
This information is not intended to replace the advice of a medical professional. You should always consult your doctor before making decisions about your health.